ECG Monitoring
There are several different types of ECG monitoring, including:
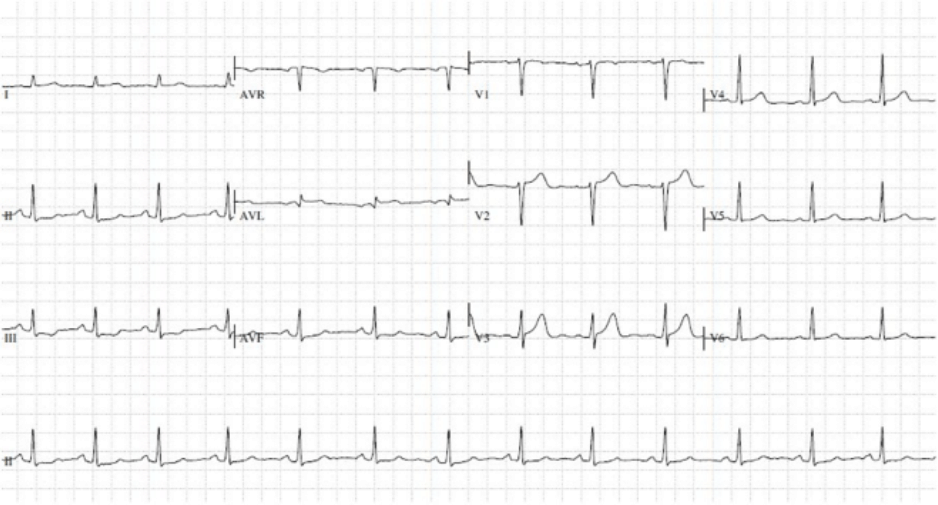
12 lead ECG
An ECG is a tracing of the electrical activity of the heart. The test is completely painless and takes only a few minutes; it involves sticking a number of small patches (electrodes) to the arms, legs and chest, which are connected by leads to an ECG machine which records the electrical impulses generated by each heartbeat. The ECG is a very useful and simple baseline test that can help to identify many different heart problems, including changes in heart rate and rhythm, a propensity to certain rhythm disturbances, abnormalities of the heart muscle and damage to the heart from a prior heart attack.
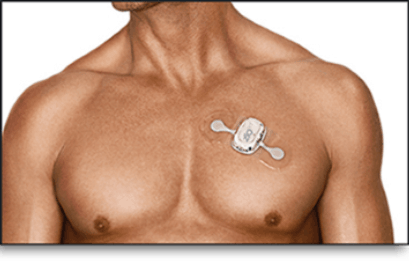
24 hour and longer term (7 and 14 day) ECG monitoring
Recording the electrical activity of the heart over a longer period of time than a standard ECG can help to identify the heart rhythm at times of symptoms such as palpitations or dizziness, which may not occur all the time. In the last few years technology has come on a long way and the former cumbersome monitors with multiple cables and stickers have been replaced with devices which come as a single unit adhesive patch and are very discreet.
It takes just a few minutes to fit the device and once it has been applied the patient should go about all their daily activities as usual until the monitoring period has come to an end, but should avoid immersing the device in water. The devices are splash-proof so a quick shower each day does not pose a problem, but patients are asked to avoid swimming and to keep the monitor above the waterline if having a bath. Saunas and steam rooms should also be avoided since these may cause the adhesive to weaken and make the patch more likely to detach from the skin.
The patient will also be asked to keep a diary of any symptoms experienced during the time the monitor is worn, so that the doctor can pay special attention to the recordings made at those times and determine whether the symptoms in question are related to the heart. The type of device and length of recording chosen will depend on the frequency of the patient’s symptoms.
A patient might also be asked to wear a monitor for a period of time if their 12 lead ECG shows changes to the conduction system of the heart. The patient may not necessarily be aware of these changes but a longer ECG recording will help the doctor to determine if any treatment is required to manage them.
Event recorder
For very infrequent symptoms which have not been detected on continuous monitoring, a patient might like to consider use of an event recorder, such as the Kardia AliveCor, which is a freestanding device activated by the patient only at the time of symptoms. This type of monitor is a small hand-held device that the patient simply carries around with them or attaches to their smartphone. At the time of symptoms the patient touches the metal feet on the monitor with their fingers to generate an ECG trace. There is also a strap that attaches to an Apple watch which allows it to take ECG traces. These can then be forwarded to a doctor for analysis.
Implantable Loop Recorder (ILR, Reveal device)
If a patient has very troublesome but infrequent symptoms, for example feeling faint, severe palpitations or loss of consciousness, it is highly likely that short-term monitoring will fail to pick up the underlying abnormality. In these circumstances it may be appropriate to use an implantable loop recorder (ILR) such as the Reveal™ Linq device. This is a compact but highly sophisticated device, smaller than an AAA battery (as pictured for comparison), which is inserted under the skin on the front of the chest. This is performed as an outpatient procedure, taking around half an hour, and requiring only a local anaesthetic.

The device automatically records any abnormal heart rhythms, and the patient can also activate it at the time of symptoms. It is activated using a small hand-held device which is placed on the skin overlying the device; pressing the button on the activator stores the ECG for a set period of time before, during and immediately after the activation. The data can then be downloaded during a device check in clinic, or remotely through the CareLink system, which allows patients to transmit their data using a 3G data card.
By looking at automatically stored and patient stored ECGs it is possible to determine whether or not a patient’s symptoms are due to significant changes in the heart rate and rhythm. Once a diagnosis has been made, or if it becomes clear that there is not an underlying heart abnormality, the ILR is removed under local anaesthetic. If it has been shown that the symptoms are due to inappropriate slowing of the heart a permanent pacemaker can be inserted at the same time.
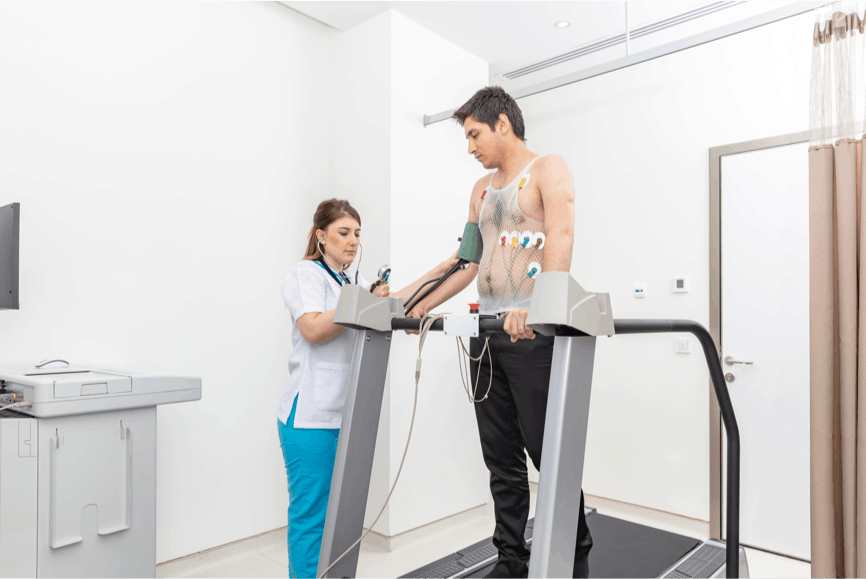
Exercise Tolerance Test (ETT, treadmill test)
An exercise tolerance test, sometimes called a stress ECG or treadmill test, is an ECG carried out while the patient exercises, usually on a treadmill but sometimes on a stationary bicycle. Pain or other symptoms brought on by exercise can be indicative of a specific type of pain or discomfort caused by coronary artery disease. An exercise ECG can therefore help to diagnose coronary heart disease, and in patients already known to have this condition it can give more detailed information about the severity of the illness and help doctors to establish a treatment regimen. The test usually takes about half an hour, beginning at a very easy rate and gradually made harder by increasing the slope and speed of the treadmill. The ECG tracing and blood pressure will be monitored constantly by a doctor and a technician, and readings will continue to be taken in the recovery period after exercising. The test can be stopped at any time if the patient develops any chest pain, breathlessness or fatigue. Comfortable clothing and shoes suitable for exercise should be brought along for the test.

Related links:
Symptoms - Palpitations, dizzy spells and
blackouts
Palpitations are a common symptom that may or may not signify an important underlying heart problem. Read more
Conditions - Atrial Fibrillation
Atrial fibrillation (often abbreviated to “AF”) is a very common heart rhythm disturbance, affecting over a million people in the UK. Read more
Conditions - Other Arrhythmias
For the heart to beat effectively the heart muscle cells must contract in an organised and predetermined way. Read more
Medical Therapy - Atrial Fibrillation
When the atria fibrillate, they no longer contract in a mechanically useful way, causing a degree of stagnation to blood flow and predisposing to clot formation within the chambers, and in particular within a finger-like projection called the left atrial appendage. Read more
Treatments - Ablation
The role of ablation in the treatment of various abnormal heart rhythms has evolved over the last two decades and now has an established place in the management of various arrhythmias, the most common of which is atrial fibrillation. Read more